Secure Smart payments
Enhancing Health Data Collection in Appalachia
By Bridging Technological and Cultural Gaps
In the remote areas of Appalachia, gathering accurate health data posed a significant challenge due to varying literacy levels and limited technological literacy among the population. The University of Pittsburgh and the University of West Virginia undertook a longitudinal health study in this region, aiming to collect comprehensive health data through self-report surveys. However, the traditional method of using bubble sheets for data collection proved to be inefficient, error-prone, and inaccessible to many participants. This case study explores how a mobile app was developed to overcome these challenges, significantly improving data collection efficiency, reliability, and participant engagement.
The development of the mobile app spanned over four months, focusing on creating an inclusive and user-friendly solution that catered to the unique needs of the Appalachian community. Through a series of interviews, observations, and iterative testing, the app was designed to include audio and tactile options for survey completion, enabling participants to engage with the health study privately and at their own pace. This initiative not only revolutionized the data collection process but also empowered the community by making health research more accessible and inclusive.
The Problem
Digitizing Data in a Low-Literacy Landscape
The primary challenge was transitioning from paper-based surveys to a digital format in a region with low literacy and limited tech literacy. Key issues included:
- Participants had low reading levels and struggled with complex academic research questions.
- Surveys consisted of 119 questions, making them time-consuming and overwhelming.
- Participants needed to answer additional questions for their young children.
- Participants did not feel valued by the research staff.
- There was a significant trust issue between participants and clinic staff.
- Lack of reliable internet connectivity in remote areas hindered data collection and transfer.
- Human errors and delays in data transcription compromised data reliability.
The Solution
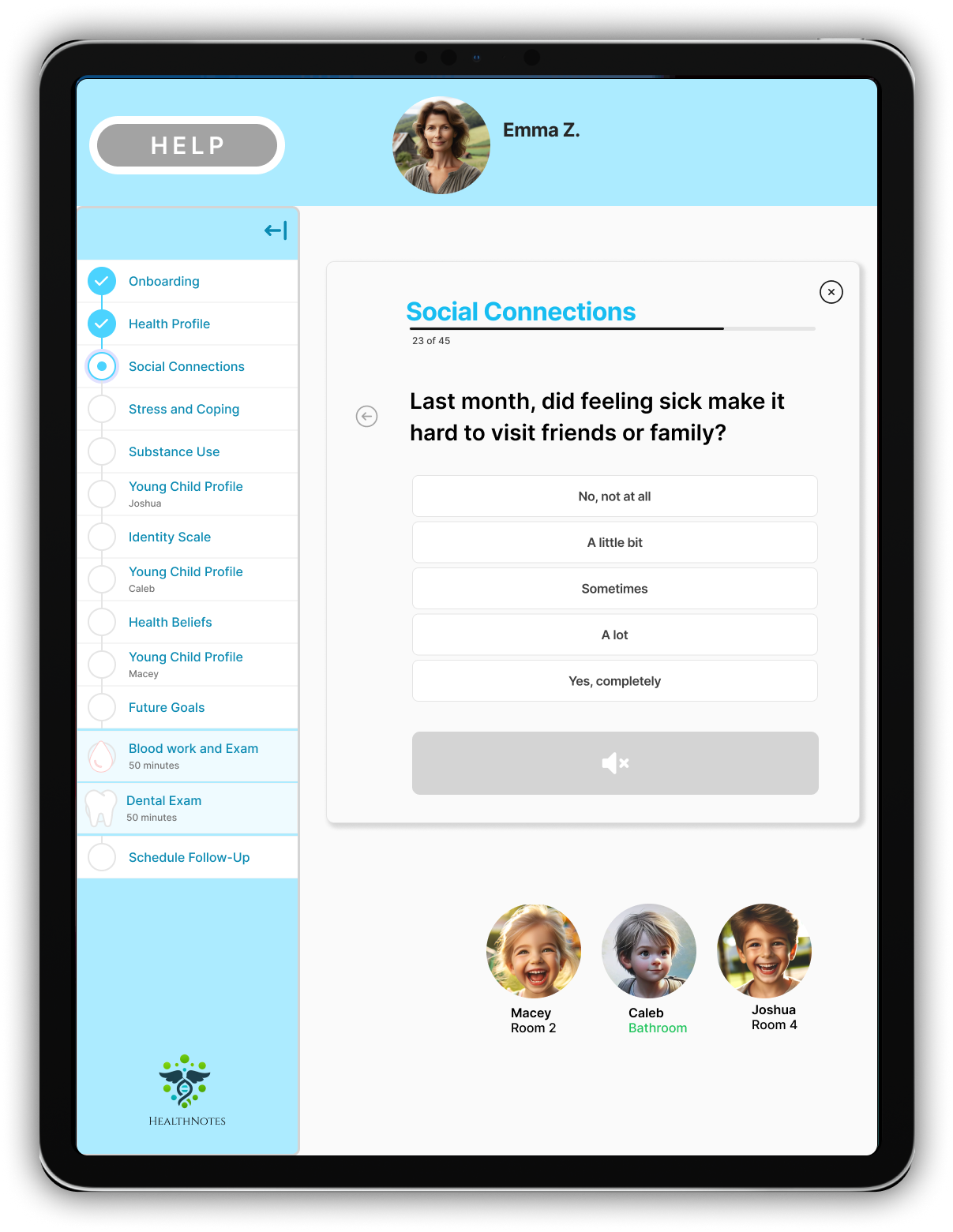
A Conversational, Voice-Guided App
To address these challenges, a tablet app with speech recognition and offline capabilities was developed. The app featured a conversational interface, enabling users to engage with health surveys orally. Key features included:
- Speech recognition for oral survey responses.
- Offline capabilities to accommodate remote areas with unreliable internet.
- Medical exam reminders to encourage participant engagement.
- Simplified question wording to enhance understanding.
- Breaks between survey sections to reduce participant fatigue.
- Save and exit options for user convenience.
- Consolidated reports for parents to fill out child-related questions efficiently.
- Enhanced speech clarity for better user comprehension.
Information Architecture
Organizing for Accessibility and Efficiency
The app's information architecture was meticulously designed to ensure a seamless user experience. Key elements included:
- A clear and intuitive user flow to guide participants through the survey process.
- Empathy maps and personas to understand user needs and preferences.
- Task analysis to identify and streamline key interactions.
- A grid system for consistent and clean design.
- Accessible navigation options to enhance usability.
- Summary pages for users to review their medical exam results.
Value of the Project
Empowering Users and Enhancing Research
The app's development brought significant value to both users and the research project. Benefits included:
- Participants could complete surveys privately and at their own pace.
- Audio and tactile options made the app accessible to individuals with vision impairments or reading disabilities.
- The app increased participant engagement and confidence.
- Data collection became more efficient, with data available within 12 hours instead of weeks.
- Enhanced data reliability due to reduced human errors and participant gaming.
- Improved participant-trust through employing local staff and empathetic design.
- Full funding for the project was secured due to the app's success.
UI Design
User-Centered and Accessible
The user interface design focused on accessibility and user-friendliness. Key aspects included:
- A conversational interface to guide participants through surveys.
- Large, clear buttons and text for easy navigation.
- Audio cues and instructions for users with reading difficulties.
- Color contrasts and intuitive layouts to enhance visual clarity.
- Offline functionality to support data collection in remote areas.
Conclusion
Overcoming Barriers with User-Centered Design
This project demonstrates the transformative impact of user-centered design in overcoming literacy and cultural barriers in product design. The mobile app's development not only improved data reliability and collection efficiency but also empowered the Appalachian community by making health research more accessible and inclusive. Looking ahead, further refinements to the app will continue to broaden its reach and efficacy.
The importance of thoughtful design and real-world testing in creating solutions that truly meet user needs. By leveraging technology and empathetic design principles, the app successfully bridged the digital divide in health data collection, setting a precedent for future initiatives in similar contexts.
